MCH (Mean Corpuscular Hemoglobin) – the average hemoglobin content in the red blood cell
MCH is a measure that reflects how much hemoglobin is contained on average in one red blood cell. It helps to assess the ability of the blood to carry oxygen and is used to diagnose various types of anemia.
Norm of MCH in the blood test
- Adults and children: 27-34 picograms (pg) per red blood cell
- Newborns: 32-36 pg (usually higher than adults)
The role of MCH in the body
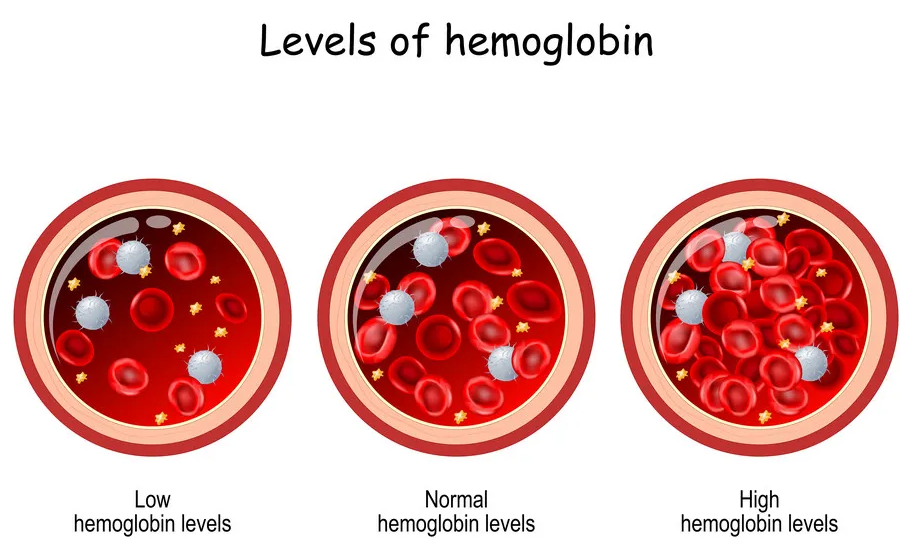
Hemoglobin is a protein that binds oxygen and delivers it to tissues. MCH shows how much red blood cells are saturated with hemoglobin:
- Normal value (27-34 pg) – red blood cells carry oxygen efficiently.
- Elevated MCH (>34 pg) – hyperchromia (excess of hemoglobin in cells).
- Low MCH (<27 pg) – hypochromia (lack of hemoglobin, most often due to iron deficiency).
Abnormal behavior: symptoms and causes
1. Elevated MCH (hyperchromic anemia)
Reasons:
- Vitamin B₁₂ or folic acid deficiency -red blood cells increase (macrocytosis) and contain more hemoglobin.
- Liver diseases – protein synthesis, including hemoglobin, is disrupted.
- Hypothyroidism -slowing down the metabolism affects hematopoiesis.
- Alcoholism is a toxic effect on the bone marrow.
Symptoms:
- Weakness, fatigue
- Pallor with slight jaundice (due to destruction of large red blood cells)
- Numbness and tingling in the extremities (with B₁₂ deficiency)
- Glossitis (inflammation of the tongue)
2. Low MCH (hypochromic anemia)
Reasons:
- Iron deficiency anemia (the most common cause) — low iron → low hemoglobin.
- Thalassemia is a hereditary disorder of hemoglobin synthesis.
- Chronic diseases (kidney failure, inflammation).
- Lead poisoning -blocks the synthesis of heme.
Symptoms:
- Weakness, dizziness
- Pale skin, brittle nails and hair
- Shortness of breath during exercise
- Picacism (strange taste preferences – the desire to eat ice, clay, chalk)
Diagnosis and treatment
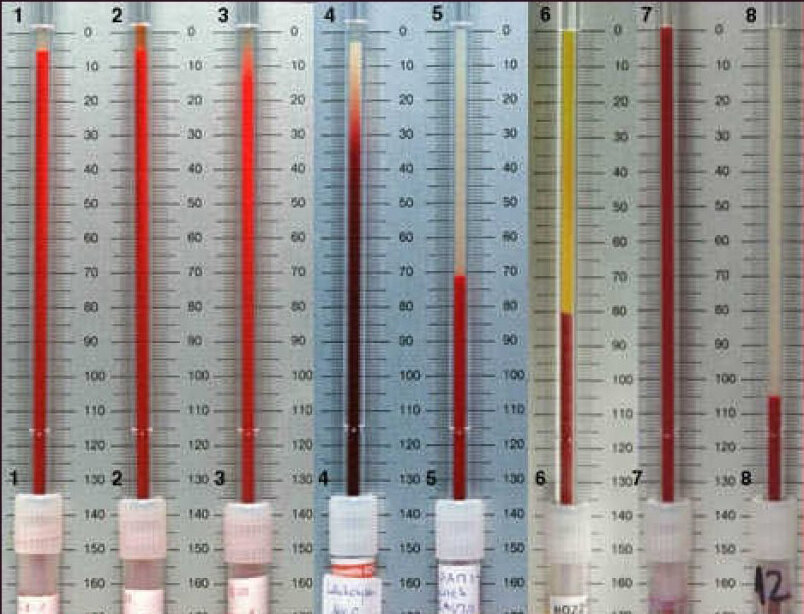
- A general blood test (UAC) is the main method.
- Additional information: ferritin, iron, vitamin B₁₂, folic acid.
- Treatment depends on the cause:
- For iron deficiency – iron supplements + vitamin C for better absorption.
- In case of B₁₂/folate deficiency – b₁₂ injections or folic acid intake.
- In case of chronic diseases-correction of the main pathology.
Important: MCH is evaluated together with MCV (red blood cell size) and MCHC (red blood cell hemoglobin concentration) to accurately diagnose the type of anemia.
Examples of interpretation:
| Parameter | Iron-deficiency anemia | Vitamin B₁₂-deficiency anemia |
|---|---|---|
| MCH | ↓ (<27 pg) | ↑ (>34 pg) |
| MCV | ↓ (<80 fL) | ↑ (>100 fL) |
| MCHC | ↓ (<320 g/L) | Normal or ↓ |