Роль TNF-α (фактора некроза опухоли-альфа) в организме
TNF-α – это провоспалительный цитокин, который играет ключевую роль в:
✔ Иммунной защите – активирует макрофаги и нейтрофилы для борьбы с инфекциями.
✔ Апоптозе – запускает гибель поврежденных или раковых клеток.
✔ Воспалении – усиливает выработку других цитокинов (IL-1, IL-6).
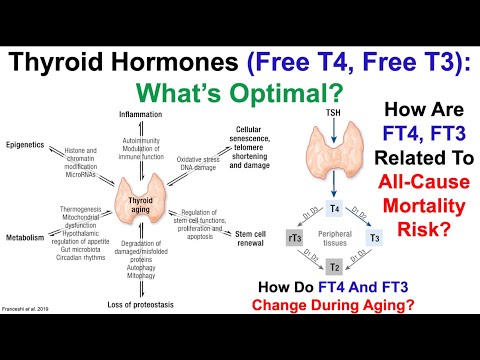
✔ Метаболизме – влияет на инсулинорезистентность и липолиз.
✔ Терморегуляции – вызывает лихорадку при инфекциях.
Симптомы и последствия дисбаланса TNF-α
При избытке (гипервоспаление)
- Острые состояния:
- Сепсис, цитокиновый шторм (шок, полиорганная недостаточность).
- Тяжелые инфекции (COVID-19, туберкулез).
- Хронические болезни:
- Аутоиммунные заболевания (ревматоидный артрит, болезнь Крона).
- Атеросклероз, диабет 2 типа.
- Депрессия, нейродегенерация (болезнь Альцгеймера).
При дефиците (крайне редко)
- Склонность к инфекциям (особенно внутриклеточным, например, туберкулезу).
- Нарушение заживления ран.
- Снижение противоопухолевого иммунитета.
Примечание: Полное отсутствие TNF-α встречается при редких генетических мутациях.
Нормы TNF-α в анализах
Уровень TNF-α измеряется в сыворотке крови методом ИФА. Референсы зависят от лаборатории, но обычно:
| Состояние | Уровень TNF-α (пг/мл) |
|---|---|
| Здоровые люди | < 8.1 |
| Легкое воспаление | 8.1–15 |
| Острое воспаление | 15–50 |
| Аутоиммунные болезни/сепсис | > 50 (до 1000+) |
Когда назначают анализ?
- Подозрение на сепсис, аутоиммунные заболевания.
- Контроль терапии биологическими препаратами (ингибиторами TNF-α).
- Оценка тяжести COVID-19, ревматоидного артрита.
Что делать при отклонениях?
При высоком TNF-α
- Медикаментозная терапия:
- Ингибиторы TNF-α (адалимумаб, инфликсимаб – при ревматоидном артрите).
- Кортикостероиды (преднизолон).
- Натуральные методы:
- Куркумин, омега-3 (снижают воспаление).
- Низкоуглеводная диета (уменьшает инсулинорезистентность).
При низком TNF-α
- Лечение основного иммунодефицита.
- Вакцинация (по показаниям).
Интересные факты
- TNF-α и рак: в низких дозах защищает от опухолей, в высоких – может стимулировать их рост.
- Депрессия: хронически повышенный TNF-α нарушает выработку серотонина.
Вывод
TNF-α – «страж» иммунитета, но при избытке разрушает ткани.
Норма: < 8.1 пг/мл (кровь).
Повышение:
- >15 пг/мл – острое воспаление,
- >50 пг/мл – риск полиорганных осложнений.
Коррекция: биопрепараты, противовоспалительная диета.
Пример: При ревматоидном артрите уровень TNF-α >20 пг/мл – показание для назначения адалимумаба.