Methylene blue (MS) is not just a dye. This is a unique substance with a 150-year history, which has turned from a remedy for the treatment of malaria into an object of close attention of modern scientists studying diseases of aging, cancer and energy metabolism.
What is methylene blue and how does it work? Molecular mechanisms
The main ‘target’ of methylene blue is the mitochondria, the energy stations of our cells. Its action can be described through several key mechanisms.
1. Alternative electron transport (‘Bypass road’)
This is the main and most studied mechanism that explains the neuroprotective properties of MS.
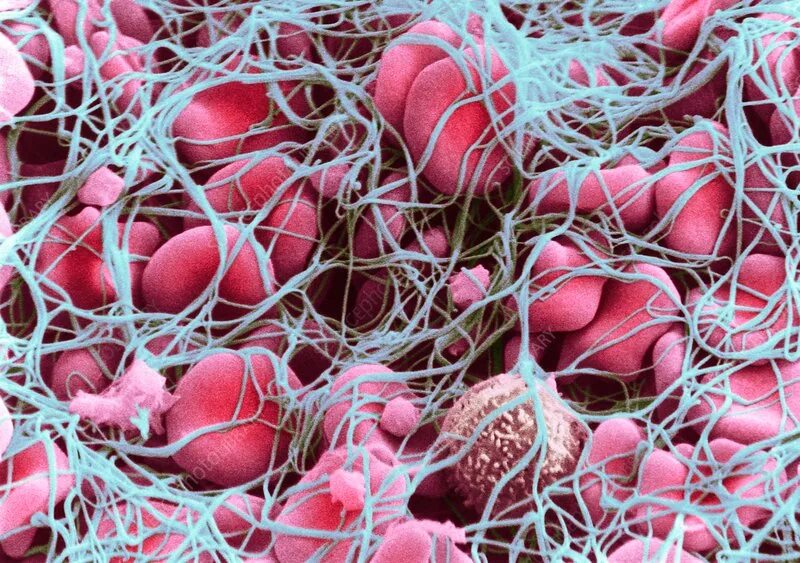
- Problem: In the respiratory chain of mitochondria, sometimes a ‘plug’ occurs — one of the protein complexes is blocked, most often the I-th. This leads to the accumulation of electrons, their ‘unauthorized’ exit from the chain and the formation of reactive oxygen species (ROS), which damage and kill cells. This is a key factor in the development of neurodegenerative diseases (Alzheimer’s, Parkinson’s).
A key target in the mechanism of action of methylene blue is the first protein complex (NADH-dehydrogenase complex) of the mitochondrial respiratory chain. This complex is the largest and most complex molecular apparatus in human mitochondria, consisting of 44 protein subunits. Because of its size and key role in electron transport, it is most vulnerable to various disturbances. When it is blocked (which can occur due to genetic mutations, the action of toxins, or age-related changes), a kind of ‘plug’is formed in the respiratory chain. Electrons coming from nutrients cannot pass further, accumulate and begin to ‘go off the track’, reacting unauthorized with oxygen. This leads to the massive formation of superoxide radical and other reactive oxygen species (ROS), which trigger oxidative stress, damage to cellular structures and, ultimately, cell death, which is especially dangerous for brain neurons. Methylene blue, acting as an artificial carrier, ‘bypasses’ this blocked complex, removing the electronic plug and preventing catastrophic consequences.
- Solution: Methylene blue acts as a’bypass road’. It takes on the’ stuck ‘ electrons and transmits them directly to Cytochrome C, bypassing the blocked site. This removes congestion and drastically reduces the production of harmful ROS.
- Result: The cell receives energy in a safer way, and neurons are protected from oxidative stress.
2. Dual Nature: Antioxidant and Pro-Oxidant
This is the most paradoxical aspect of MS. Its action depends on the context.
- In the dark (inside the body): When taken orally, MS works primarily as an antioxidant and cytoprotector, implementing the ‘bypass road’ mechanism.
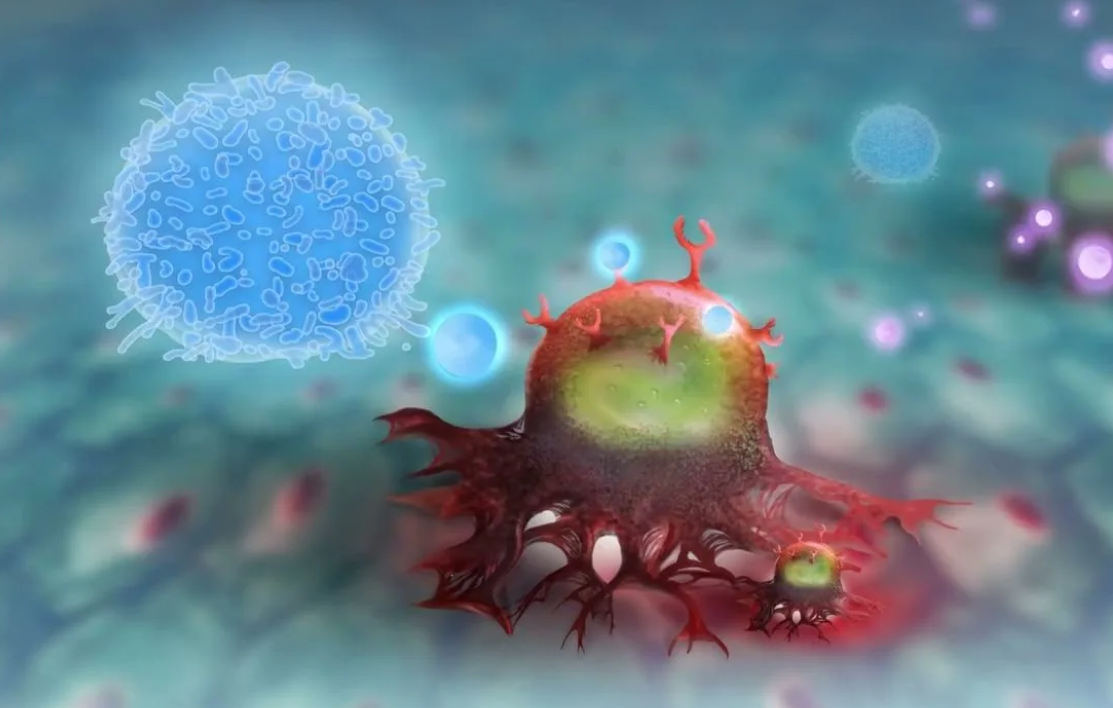
- In the light (under irradiation conditions): MS is a powerful photosensitizer. When exposed to light of a certain wavelength (red spectrum), it generates singlet oxygen — an extremely aggressive form of ROS that destroys everything in its path.
- Application: This property is used in photodynamic therapy of cancer. , delivered to the tumor and irradiated, causing the death of cancer cells.
3. Direct impact on pathologies
- Alzheimer’s Disease: MS is able to inhibit the formation and aggregation of beta-amyloid plaques — one of the main markers of this disease.
- DNA Repair: Research by Gureev’s group has shown that MS and its metabolite Azur B can trigger signaling pathways responsible for DNA repair, particularly in mitochondria. This explains its protective role in chemotherapy.
4. Impact on the microbiome
In high doses, MS exhibits antibacterial properties, which can disrupt the composition of the intestinal microbiome. Modern research necessarily takes into account the gut-brain axis, since changes in the microbiota directly affect cognitive functions.
Dosages: From therapy to toxicity
The dose determines whether the MS will be a drug or a poison. The data are primarily based on preclinical animal studies.
- Low doses (1-4 mg / kg): They were considered effective in early studies. However, current research shows that these doses may not be sufficient for a pronounced therapeutic effect in mouse models.
- Therapeutic dose (~15 mg / kg): It was at this dosage that the older mice showed significant improvements in memory and cognitive function in the Morris test. This is the dose at which the ‘bypass’ mechanism works effectively, and no serious side effects are observed.
- Toxic doses (≥50 mg / kg): At such high doses, negative effects begin to appear:
- Inhibition of cognitive functions.
- Violation of the composition of the intestinal microbiome.
- General toxic effects.
For a person weighing 90 kg, the dose of 15 mg / kg is 1350 mg.
This is equal to 135 ml of 1% solution, which is approximately 2700 drops.
This is a HUGE and POTENTIALLY DANGEROUS dose.
Toxicity: As indicated in the interview with the researcher, in mice, toxic effects (memory suppression, violation of the microbiome) began with a dose of 50 mg/kg. For a 90 kg person, this would be 4,500 mg. Our calculated dose of 1,350 mg (15 mg / kg) is in a potentially risky area, especially without medical supervision.
Liquid volume: 135 ml is more than half of a standard glass. Drinking such a volume of concentrated dye, which is also a powerful medicine, is an extreme and dangerous procedure for health.
Conclusion: The 15 mg/kg dose studied in mice is NOT INTENDED for self-administration by humans. It is used in strict preclinical research settings. Self-medication at these dosages can lead to serious side effects, including gastrointestinal damage, dysbiosis, and neurotoxicity.
A wide therapeutic window (the difference between the effective and toxic dose) makes MS a promising drug.
Important: Transferring doses from animals to humans is a complex process. These doses are indicative and are given for scientific and informational purposes.
Side effects and precautions
- Cosmetic: The most harmless, but noticeable — staining of urine in blue-green color. In rare cases, with prolonged use, a bluish tinge of the sclera of the eyes can be observed.
- Serious issues: Risk of light toxicity. Taking high doses without understanding the mechanisms can lead to unpredictable consequences.
Can I take methylene blue for prevention?
The researcher’s answer is a categorical ‘ no ‘ to self-medication.
Methylene blue is a powerful medicine, not a dietary supplement.
Preventive use of MS by healthy people is an unjustified risk. Its use should be strictly within the framework of clinical protocols under the supervision of a doctor after approval by regulatory authorities (for example, the FDA).
Prospects and conclusions
Methylene blue is a molecule with huge potential. Today, research is going in several directions:
- Neurodegenerative diseases: Attempts to conduct correct clinical trials for Alzheimer’s disease continue.
- Synergy with chemotherapy: Its ability to protect healthy tissues (kidneys, brain) from the toxicity of drugs like cisplatin is being studied.
- New analogs: Scientists are investigating MS derivatives (Uredin blue), which can be even more effective and safe.
Conclusion: Methylene blue is not a ‘mind pill’ or an elixir of youth. This is a powerful tool that deeply interferes with cellular energy. Like any powerful tool, it requires respectful and professional handling. The future of MS lies in evidence-based medicine, not in amateur activities in the style of ‘biohacking’.