Manganese is an essential traceelement that is involved in key biochemical processes:
✔ Antioxidant protection -it is a part of the enzyme superoxide dismutase (Mn-SOD), which neutralizes free radicals.
✔ Metabolism -participates in the synthesis of:
- Glucose (gluconeogenesis).
- Cholesterol and fatty acids.
✔ Bone and cartilage formation -activates enzymes that synthesize collagen and proteoglycans.
✔ The work of the nervous system -affects the transmission of nerve impulses.
✔ Reproductive health -essential for the synthesis of sex hormones.
Symptoms of manganese deficiency
Deficiency is rare, but it is possible if:
- Long -term parenteral nutrition (without Mn supplements).
- Genetic disorders of manganese metabolism.
Signs:
- Bone growth disorders (osteoporosis, scoliosis in children).
- Reduced glucose tolerance (pseudodiabetes).
- Hypercholesterolemia.
- Convulsions, tremors (due to neurotransmitter dysfunction).
- Depigmentation of the skin and hair.
Symptoms of excess manganese
Toxicity develops when:
- Chronic inhalation of manganese dust (in welders, miners).
- Genetic disorders (for example, mutations in the SLC30A10 gene ).
- Long-term intake of dietary supplements with Mn (>11 mg / day).
Signs:
- Neurological disorders:
- Manganese parkinsonism (tremor, muscle rigidity).
- Mental disorders (aggression, hallucinations).
- Liver damage(fibrosis).
- Cardiomyopathy.
Norms of manganese in analyses
The level of manganese is determined in:
1. Whole blood (the most accurate method)
| Group | Norm (mcg/l) |
|---|---|
| Adults | 4–15 |
| Children | 5–20 |
2. Blood serum
- The norm: 0.5-1.2 mcg/l.
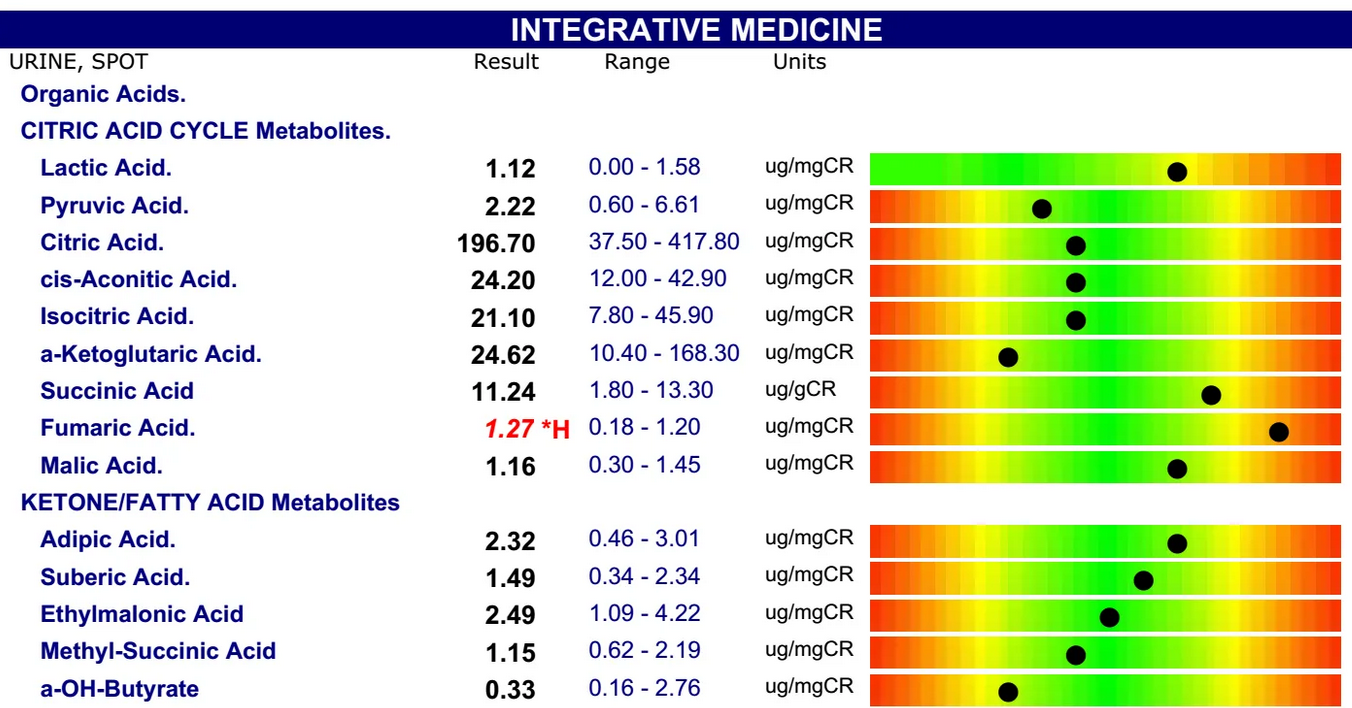
3. Urine (daily)
- The norm: < 2 mcg/day.
4. Hair/Nails
- The norm: 0.1-1.5 mcg/g.
Critical levels:
- > 20 mcg / l (blood) — toxicity.
- < 2 mcg/l (blood) — deficiency.
When are tests scheduled?
- Suspected manganese poisoning (in employees of hazardous industries).
- Neurological symptoms (Parkinsonism of unknown origin).
- Osteoporosis or growth disorders in children.
- Control of parenteral nutrition.
What should I do if there are deviations?
If there is a shortage:
- Diet: nuts (hazelnuts, pecans), whole grains, pineapple, spinach.
- Supplements: manganese gluconate (2-5 mg / day).
If there is an excess:
- Chelation therapy (EDTA, dimercaprol).
- Avoid contact with manganese dust.
- Iron intake (reduces the absorption of Mn).
Examples of interpretation
- Blood manganese = 25 mcg / l + tremor → poisoning, chelation required.
- Blood manganese = 1 mcg / l + osteoporosis → deficiency, supplements are needed.
Conclusion
Manganese is a vital element for antioxidant protection, metabolism, and the bone system.
Rules:
- Blood: 4-15 mcg/l,
- Urine: * * <2 mcg / day**. * * * * * Deficiency leads to osteoporosis, neurological disorders. * * * Excess** (>20 mcg/l) causes Parkinsonism and liver damage.
Лечение *Treatment*: diet, chelators (for poisoning), supplements (for deficiency).